The pandemic has had a disproportionate impact on Native nations in the US with COVID-19 rates 350 percent higher among Native Americans compared to whites. In new research Raymond Foxworth, Laura E. Evans, Gabriel R. Sanchez, Cheryl Ellenwood, and Carmela M. Roybal contextualize the history of colonization and policy neglect by federal and state governments to explain the unequal impact of the pandemic. They find that this disparity is related to a lack of basic infrastructure like safe running water, a shortage of health information available in Native languages, and the high rate of non-tribal members visiting tribal lands during the pandemic. State-level partisanship also plays an important role; Republican dominated states were less likely to implement pandemic mitigation policies such as mask mandates, which in turn has put Native American lives in danger.
The first large-scale COVID-19 outbreak in a Native American community originated from a large church gathering around March 7, 2020 in the small community of Chilchinbeto, Arizona on the Navajo Nation. Like many other Native nations across the US, the Navajo Nation responded to the COVID-19 outbreak by issuing a state of emergency and closing tribal offices and businesses in an effort to stop the spread of COVID-19. By spring 2020, new cases of the coronavirus began to emerge in other Native nations across the US, and by August 2020, the US Centre for Disease Control and Prevention (CDC) reported that Native Americans had 3.5 more COVID-19 cases than White Americans and hospitalization rates five times that of White Americans.
To understand the disproportionate impact of the pandemic on Native communities, our research contextualizes the history of colonization and policy neglect by federal and state governments to show the compounding effects of COVID-19 on Native peoples. Our work provides insight into the structural and partisan causes of COVID-19 spread across Native communities during the early days of the COVID-19 pandemic in 2020.
Understanding Native Nations in the US
There are 6.9 million American Indians and Alaska Natives in the US and 574 federally recognized Native nations. Native nations are sovereign governments that vary in size, geographic location, economies, and government structure. Likewise, all Native nations vary by culture, language, and religion. Tribal homelands once spanned across all 50 states. Today Native nations have landholdings in 34 states, encompassing 56.2 million acres held in trust by the US government and another 43 million acres in Alaska under the Alaska Native Land Claim Settlement Act. As sovereign nations, Native nations have distinct relationships with other American governments. The federal government is legally defined as a trustee of Native nations and has a responsibility to provide social services, healthcare, education, public safety, and land, while recognizing inherent sovereignty of Native nations.
But the federal government has failed to fulfill its trust responsibilities jeopardizing the health and well-being of Indigenous people across the North American continent. Consequently, Native Americans are disproportionately affected by high rates of poverty, unemployment, and health disparities resulting from centuries of harmful federal and state policies. Structural inequities like poor infrastructure, food insecurity, a lack of internet access, trauma, and health interventions not adapted to local context are well documented and continue to effect Native nations today.
A history of colonialism and epidemics for Native Americans
The coronavirus is a repeat of prior disease outbreaks on tribal lands. In fact, colonization is the largest health epidemic that has led to the greatest loss of Indigenous life across the Americas. For example, 90 percent of Indigenous life was lost across the Americas during the first century of European contact and death was incited by disease, starvation, and extreme poverty. Native American communities have also been disproportionately affected during more traditionally defined health epidemics. During the influenza outbreak of 1918–1919, nearly 25 percent of Native Americans caught the flu and were four times more likely to die from it compared to those living in urban areas. Similarly, in 1993, the first victims of the hantavirus outbreak in the southwestern United States were Navajo. Reflecting the racialization of health inequalities facing tribes, news agencies’ stoked fears of the unknown virus, commonly referring to it as the “Navajo flu.” During the 2009 H1N1 outbreak, American Indian and Alaska Natives’ death rates were four times greater than all other racial and ethnic groups combined in states with high Native populations.
Structural Inequalities and Partisanship Impact the Spread of COVID-19 in Native Nations
We used data from a variety of sources to examine the Native American community-level and state-contextual factors associated with the spread of COVID-19 in Native communities in the continuous US. We find that measures of political and policy marginalization, including the absence of household plumbing and access to culturally relevant public health information helped fuel the spread of COVID-19 in Native nations. Our findings accord with existing scholarship on Native and health politics in the US federalist system more broadly. Native American health outcomes are shaped by multiple layers of inequality.
Adequate access to household water remains a significant challenge for many Native nations. A lack of basic infrastructure makes it difficult to deliver both running water and safe and clean groundwater. 13 percent of Native American households in Native nations lack safe water and many others lack solid waste disposal and sewers.
A shortage of health information available in Native languages adds another layer. The lack of lifesaving information about the severity of COVID-19’s health threats, as well as best practices to reduce the spread of the virus and manage infections but English only dissemination produce language barriers. A large segment of the US population who speak a language other than English at home includes Native people who speak over 169 Indigenous languages. Over 25 percent of Native people report speaking a Native language.
“Gas mask” (CC BY 2.0) by HockeyholicAZ
Our research also identifies that the high rate of non-tribal members visiting tribal lands during the pandemic endangered the health and safety of tribal people on their homelands. As Katherine Florey of UC Davis has documented, COVID-19 has exposed the consequences of longstanding federal limits on tribal governments’ ability to regulate non-tribal members when they endanger health and safety on tribal lands.
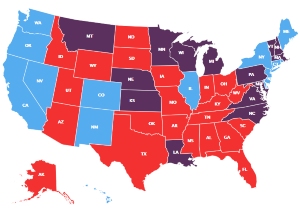
Beyond community factors, we find that state-level partisanship is associated with COVID-19 spread in Native nations: Native nations in Republican states experience higher COVID-19 infection rates, as do states with higher ratios of Trump voters in their borders. Policy differences based on partisanship at the state and local level are well established. For example, as of early August 2020, 32 US states required face coverings statewide: 24 were led by Democratic governors who have issued a mask mandate and only eight states run by Republicans implemented a mask mandate. Furthermore, Democratic states were quicker to implement mask wearing policies, with half of the Democratic-led states having mandates in place by March 2020. Former President Trump consistently downplayed the dangers of COVID-19, disparaged public health policies that can reduce the spread of the disease, and pressured Republican governors to avoid utilizing their powers to protect public health. Combined, we find that these behaviors endangered Native American lives and furthered the spread of the virus.
More investment in infrastructure and healthcare in Native Nations is needed
A number of policy recommendations emerge from our research. There must be greater prioritization and investment in infrastructure on tribal lands (i.e., safe drinking water, quality housing, electricity, broadband) by the federal government. This has been a consistent call by bipartisan federal commissions. Greater investment must also be made in growing the healthcare capacity of Native nations including investment in greater quality access, culturally relevant healthcare practices, capacity to respond to health crises and increasing tribal stockpiles for lifesaving equipment and personal protective equipment. The right to quality healthcare is a treaty right of Native nations and the federal government must honor these treaties and their relationship with Native nations in the US. Finally, both federal and state governments, as well as American citizens, must recognize the inherent sovereign rights of Native nations and respect their policy decisions passed to protect their tribal citizens.
- This article is based on the paper, ‘“I Hope to Hell Nothing Goes Back to The Way It Was Before”: COVID-19, Marginalization, and Native Nations’ in Perspectives on Politics.
Please read our comments policy before commenting.
Note: This article gives the views of the author, and not the position of USAPP – American Politics and Policy, nor the London School of Economics.
Shortened URL for this post: https://bit.ly/3hGsqNj
About the authors
 Raymond Foxworth – First Nations Development Institute
Raymond Foxworth – First Nations Development Institute
Raymond Foxworth is Vice President of First Nations Development Institute, a national Native American controlled nonprofit and visiting scholar at the University of New Mexico.

Laura E. Evans – University of Washington
Laura E. Evans is Associate Professor at the University of Washington’s Daniel J. Evans School of Public Policy and Governance.
 Gabriel R. Sanchez – University of New Mexico
Gabriel R. Sanchez – University of New Mexico
Gabriel R. Sanchez is a Professor of Political Science at the University of New Mexico, and UNM’S Center for Social Policy Director.
 Cheryl Ellenwood – Washington State University
Cheryl Ellenwood – Washington State University
Cheryl Ellenwood is a Scholarly Assistant Professor at Washington State University at the Center for Native American Research and Collaboration and the Institute for Research and Education to Advance Community Health.
 Carmela M. Roybal – University of New Mexico
Carmela M. Roybal – University of New Mexico
Carmela M. Roybal is a Doctoral Candidate in the Department of Sociology at the University of New Mexico.