 Whether on control and management, developing immunity, social impacts, or the role of leadership, Latin America’s exposure to Old World diseases with the arrival of Europeans holds many lessons for today’s coronavirus crisis, writes Linda Newson (Institute of Latin American Studies, University of London).
Whether on control and management, developing immunity, social impacts, or the role of leadership, Latin America’s exposure to Old World diseases with the arrival of Europeans holds many lessons for today’s coronavirus crisis, writes Linda Newson (Institute of Latin American Studies, University of London).
Earlier in my career I wrote extensively on the devastating demographic impact of Old World diseases in colonial Latin America following the arrival of Europeans. While we now have greater knowledge of how diseases spread and how to control them, in the current COVID-19 crisis I am constantly reminded how many of the issues we face today have parallels with those that I studied the past.
Epidemic diseases through the centuries
Epidemic diseases that result in high mortality have one feature in common: they all have their origins in animals, normally domesticated animals. Hence, smallpox is related to cowpox, influenza to swine flu, and measles probably to rinderpest and/or canine distemper. It has been suggested that COVID-19 may have originated in bats and perhaps spread to humans via a pangolin in a wet market in Wuhan, China.
When new diseases emerge, they cause high mortality because most humans lack immunity due a lack of previous exposure. This scenario has been repeated multiple times in the past, beginning in the Christian era when populations in China, India, and the Mediterranean grew sufficiently large to sustain acute infections. With the development of transoceanic trade and colonial expansion from the 15th century, their incidence increased dramatically.
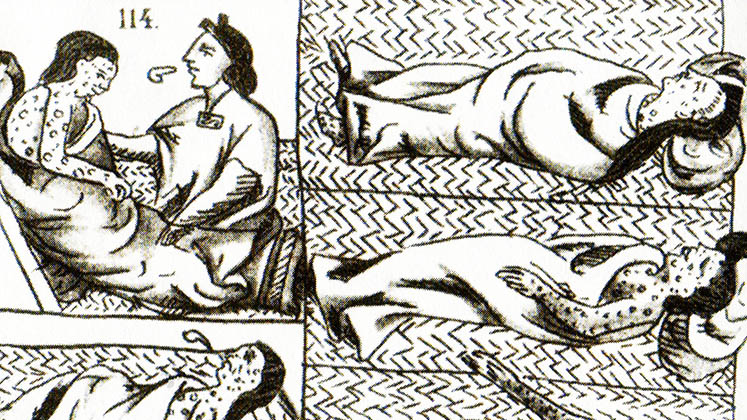
Those regions most profoundly affected at that time were those that in the pre-colonial era had been relatively isolated, notably the Americas, Australasia, and the Pacific islands. The extent of the demographic impact of acute infections in the 16th century has been debated, but it has been suggested that in the Americas the population may have been reduced to one tenth of its previous size. Even those who dispute the level of demographic collapse agree that disease was a major cause, and most accept that a single epidemic like smallpox could cause 20 or 30 per cent mortality.
While the initial impact of acute infections on non-immune populations is generally accepted, my research suggested that it is difficult to generalise about their spread and impact. Pathogens themselves differ significantly in the way they spread, for how long they remain infectious, and what environmental conditions they require to survive. A parasite may depend on an insect or animal vector to reach a new host or rely on direct contact, while all have environmental limits beyond which they cannot survive. Mosquitos causing malaria, for example, can only survive in warm climates.
Parasites themselves also change over time, and this is especially true of viruses, such as those that cause influenza, which mutate more rapidly than other pathogens. Although caused by a bacterium rather than a virus, it is thought that the incidence of once-deadly scarlet fever declined due to changes in the pathogen itself. Every parasite has its own history.
In modelling the spread and impact of acute infections epidemiologists have recognised the importance of population size and density as crucial factors. However, less explored, especially historically, has been the influence of the economic and socio-political characteristics of the society into which it is introduced. This may not only affect the spread of a disease, but also a society’s ability to develop immunity to it and recover. History has demonstrated that these cultural influences can result in considerable geographical variations in the impact of a single epidemic.
This is a large topic, which I have explored in several books and papers, particularly in the context of the colonial experiences of Central America (especially Honduras and Nicaragua), Ecuador, and the Philippines. Here I will focus on two issues that seem particularly pertinent to the COVID-19 pandemic. These are the significance of cultural factors in enabling societies to develop immunity to a pathogen and the importance of leadership in crisis management.

Developing immunity
Some individuals have innate immunity that derives from their genetic, bio-chemical, or physiological make-up, but most people acquire it through exposure to an infection. Acquired immunity cannot be inherited, so historically a society could only develop immunity where the parasite remained in the community and continually infected susceptible individuals. Today, it is more often induced through vaccination.
A pathogen needs to reach a suitable host within a specified time, which if it does not, dies out. Acute infections associated with epidemics are only infectious for short periods, so they can only circulate where populations are large or there are intense contacts with an external source of infection. However, the period for which a disease is infectious varies, and the shorter the infectious period, the higher the chances of a “fade out” occurring.
Epidemiologists have calculated that for measles – infectious for eight days – to become endemic, it is necessary to have a population of between 200,000 and 300,000, or even 500,000, in order for it to be able to generate 7,000 “susceptibles” in the form of children to maintain the parasite. On the other hand, smallpox remains infectious for two weeks and can survive on clothing and bedding for up to eighteen months; it therefore has more time to find a new host. As a consequence, smallpox is associated with a lower threshold population of 200,000, which helps to explain why during the first century of European presence in the Americas, smallpox epidemics were more frequent than those of measles and especially influenza.
The ability of a society to develop what epidemiologists have called “herd immunity” thus depends on the size and density of the population, as well as the intensity of outside contacts. However, it also depends on the fertility rate that produces a new generation of non-immune hosts in the form of children.
Evidence from colonial Andes suggests that epidemics resulted in reduced fertility as marriages were broken up by partner death or flight, as economic conditions deteriorated and the psychological effects of an epidemic encouraged smaller families. Evidence from colonial Ecuador suggests that it took about one hundred years for the population to acquire “herd immunity”, such that smallpox and measles become diseases of childhood.
It is worth noting that in pre-industrial non-contracepting societies, due to high mortality and low life expectancy, population growth is not normally more than one per cent a year. Even a small change in fertility can therefore affect a society’s ability to recover demographically. The current dilemma, which is many respects parallels the colonial experience, is that in the absence of vaccines “herd immunity” can only be acquired through continued exposure that results in high mortality over an extended period. Such a strategy has probably never been socially and politically acceptable, but it is perhaps even less so today given our greater knowledge of how epidemics operate and can be controlled.
Where populations are small and the fertility rate is low, “fade outs” often occur. These small societies are therefore unable to acquire immunity, and any re-introduction of the disease results in high mortality. Hence the impact of the same disease may be different according to the characteristics of the society and at different points in time.
For Ecuador I have argued that populations in the highlands were able to develop immunity to a number of acute infections and recover at an early stage, with some becoming endemic by the beginning of the 17th century, whereas societies in the Amazon headwaters continued to suffer high mortality due to reinfection at regular intervals throughout the colonial period. This resulted in a continued decline that was only effectively reversed with the introduction of scientific medicine in the twentieth century. Nevertheless, the lack of immunity amongst Amazonian populations makes them particularly susceptible to new infections even today.

Disease control and management in history
During the current COVID-19 pandemic, many states have sought to contain the disease through confining people to their homes to reduce social contact. Historically, quarantining was used as a method of inhibiting the spread of an epidemic, as with bubonic plague and leprosy, though measures generally focused on improving sanitary methods rather than reducing levels of contact. Quarantining might be effective where diseases are spread through face-to-face contact, but not where they are spread by an animal vector such as a mosquito or rat.
However, in the past, and as we are seeing today, when a new pathogen emerged, knowledge of how it is spread was limited, so that many measures taken were inappropriate and did little to contain the infections in question. For diseases spread though face-to-face contact, population density and distribution clearly influenced the initial impact of disease, but the nature of interpersonal contacts was also affected by a range of cultural factors. These may include the extra-communal trade and travel, religious pilgrimages and congregations, bathing practices, or residence in extended- rather than nuclear-family households.
Less frequently discussed in the literature is how cultural factors may influence the ability of a society to recover from an epidemic, which also varies according to the cohort affected. The death of able-bodied adults has a much greater impact on recovery, especially where those dying possess specific and scarce skills. In the colonial Andes, where the indigenous population may have been reduced to just a tenth of its size in the sixteenth century, this led to the widespread abandonment of irrigation works, terracing, and raised fields. Large scale losses can also affect food supplies and result in reduced levels of nutrition. The death of fertile women can also result in an immediate loss of reproductive capacity that cannot be restored until a new generation of reproductive women emerges. Where only one partner dies, demographic recovery may also be held back by opposition to remarriage and/or by marriage rules that determine the suitability of spouses, factors which are more significant in smaller communities where marriage pools are small.
Leadership can play a critical role in determining the way the crisis is managed and therefore also its outcomes. State societies generally have greater administrative capacity to organise practical responses. However, where leadership is weak or a leader dies or fails to command confidence in the measures being taken, this can lead to social unrest and conflict. This can be illustrated most dramatically in the death of the Inca ruler, Huayna Capac, probably from smallpox, around 1524, which precipitated a widespread dynastic civil war between his sons Huascar and Atahualpa. This war, together with the Inca wars of conquest, is estimated to have cost 100,00 lives before the Spanish arrived. In addition, where the cause of a disease is unknown and there is a lack of strong leadership, blame is often placed on an outside group or class, leading in the case of Amazonian groups to intertribal conflict and increased mortality.
Overall, It is clear that each new disease poses multiple questions, some of which relate to the nature of the disease itself, its infectiousness, how it is spread, and who it infects. Scientists are learning more about the characteristics of COVID-19 as it spreads. However, we should expect that the impact of the disease, and indeed a society’s ability to recover, will not be the same throughout the world. History demonstrates that cultural factors, including the actions taken by leaders, will be important factors in explaining geographical variations in the impact of pandemic diseases.
Notes:
• The views expressed here are of the authors rather than the Centre or the LSE
• This article was first published via the ILAS Latin American Diaries blog
• This piece is reproduced courtesy of the author; Creative Commons does not apply
• Please read our Comments Policy before commenting





